Infection Mechanism of Giardia
1.Localization and Diagnostic Challenges:Giardia primarily parasitizes the small intestine. During chronic diarrhea infections, trophozoites are rarely excreted in feces, making microscopic detection of trophozoites clinically insignificant for most of the infection cycle.
2.Encystation and Transmission: A small number of trophozoites may migrate to the large intestine during infection. To survive in the external environment for waterborne transmission, these trophozoites rapidly form hardy cysts within 24 hours(Cysts are resistant to nucleic acid extraction, leading to potential false-negative PCR results). Additionally, when present in low numbers, cysts may be easily overlooked under the microscope due to suboptimal viewing fields or angles, or may be misidentified as yeast-like structures.
3.Large quantities of trophozoites or cysts are only occasionally observed in feces. During acute gastrointestinal issues or diarrhea, trophozoites from the small intestine may be expelled.In the late stage of infection, when the small intestine is saturated, Giardia releases large numbers of trophozoites or cysts to facilitate host-switching.
Principle of Accuracy in New Test Fluorescent Immunoassay
Immunoassays detect proteins and do not require the presence of intact cells. Throughout the entire infection cycle, Giardia lamblia undergoes continuous proliferation and death, releasing large amounts of protein fragments into the feces via the digestive tract. These protein fragments are invisible under microscope, and nucleic acids from lysed cells are readily degraded in the digestive tract. The immunoassays can accurately reflect the current parasitic load of Giardia in the small intestine.
1.Targeting Soluble Antigens (Independent of Intact Parasites)
Detection Targets: Specific proteins of Giardia lamblia (e.g. GSA-65, α-1 giardin, etc.), no intact cells required.
Advantages:
1) Even if the parasites disintegrate, its secreted or excreted protein fragments remain detectable in feces.
2) Proteins exhibit far greater stability in the intestinal environment than nucleic acids (Highly resistant to degradation by digestive enzymes).
2.Technical Advantage Comparison
|
Parameter |
Microscopy |
Immunoassay(New Test) |
|
Detection Target |
Whole cysts/trophozoites |
Parasitic protein fragments (even after cell lysis) |
|
Sensitivity |
Low (misses protein fragments) |
High (Capable of detecting picogram-level antigens) |
|
Sample Stability |
Requires fresh samples |
Low sample storage requirements (due to protein stability) |
|
Chronic Infection Detection Rate |
≤50% |
>90% |
3.Clinical Scenario Adaptability
Chronic/intermittent cyst-shedding patients: Immunoassays can capture persistently released antigens, avoiding "false negatives" in microscopy due to irregular cyst excretion.
Screening of asymptomatic carriers: Suitable for animals with recurrent abnormal stools and screening for chronic gastrointestinal diseases.
Three Core Reasons for Microscopic False Negatives
1.Limitations of Microscopy Determined by the Parasitic Characteristics of Giardia lamblia
Parasitic location: Primarily colonizes the upper small intestine (duodenum/jejunum), while fecal samples mainly reflect large intestine contents.
During chronic infection:
Trophozoites are rarely excreted with feces (unless acute diarrhea flushes the small intestine).
Cysts are only present in small quantities in the colon (transformed for transmission), making them easily missed by microscopy.
2.Biological Challenges of Cyst Leading to Microscopic Detection Difficulties
Low Parasite Load: During chronic infection, cyst counts in feces may drop as low as 10²/g (microscopy requires ≥10⁴/g for reliable detection).
Morphological interference: Cysts (8–12 μm) overlap in size with yeast (5–10 μm), and conventional methods (e.g., iodine) fail to distinguish between them.
Cysts are easily obscured by stool residues, especially in watery stools where dilution further reduces detectability.
3.Differences Between Acute and Chronic Phases
Acute diarrhea: Large numbers of trophozoites are flushed into feces (resulting in higher microscopy detection rates), though this phase typically has a short duration.
Chronic infection: Continuous parasitism in the small intestine, only small numbers of cysts are intermittently excreted in feces (resulting in reduced microscopy detection rates).
Conventional triple fecal testing with separate submissions may still miss the diagnosis (due to irregular cyst shedding).
Why Can Nucleic Acid Testing Also Miss Infections?
1. Cyst Wall Interference
The thick cyst wall (containing polysaccharide-protein complexes) reduces the extraction efficiency of nucleic acid.
2. Nucleic Acid Degradation
Fecal nucleases rapidly degrade free DNA/RNA, particularlly when sample transportation is delayed. While Nucleic Acid Testing demonstrates high sensitivity for acute infections, it may yield false-negative results in chronic infections due to low cyst loads. In contrast, immunoassays provide more reliable detection during chronic phases, as proteins are continuously released.
Summary: The Irreplaceability of Fluorescent Immunoassay
1.Targets Stable Markers: Protein antigens are more resistant to the intestinal environment than parasite morphology or nucleic acids.
2.Full-Cycle Coverage: Reflects the current parasitic status in both acute diarrhea and chronic infection.
3.Standardized Operation: Automated reading minimizes human error.
Case Sharing:
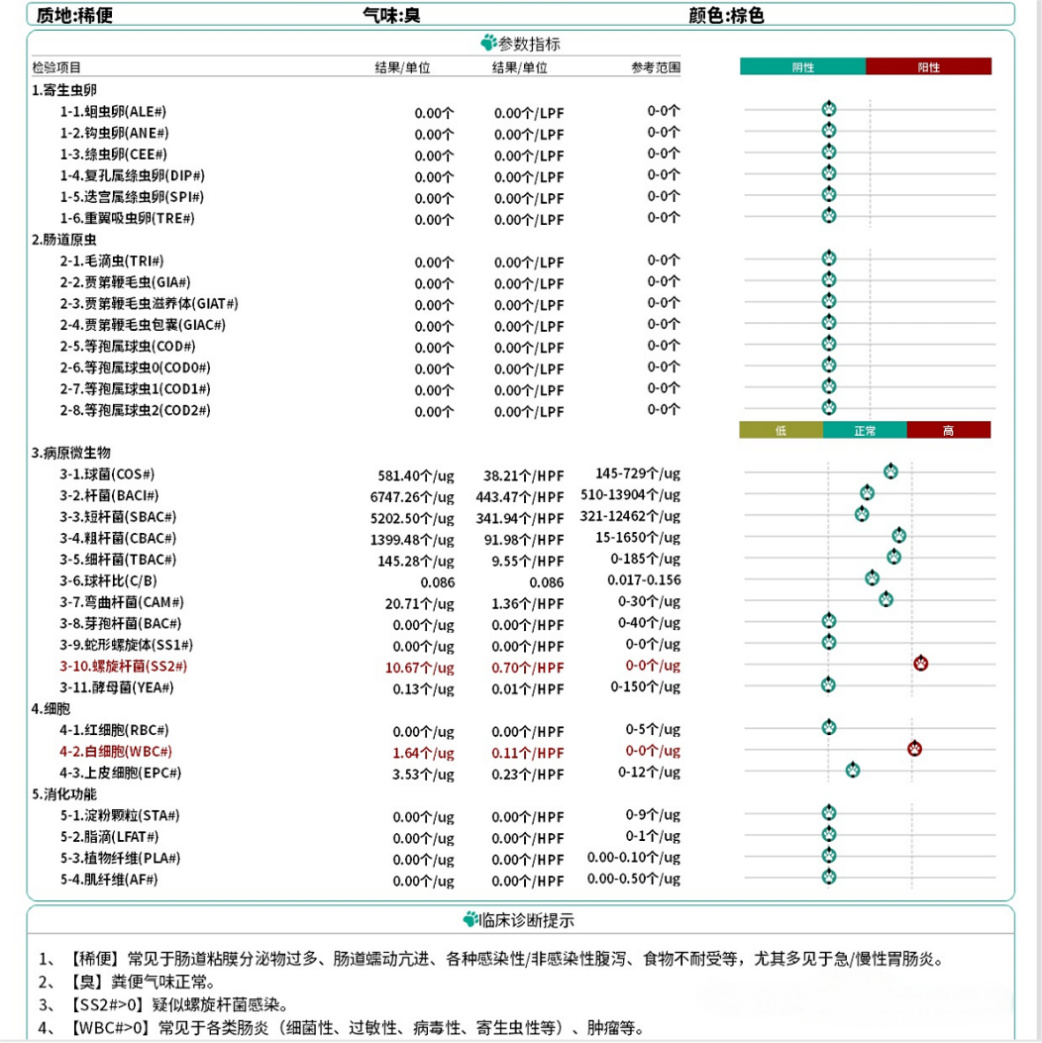
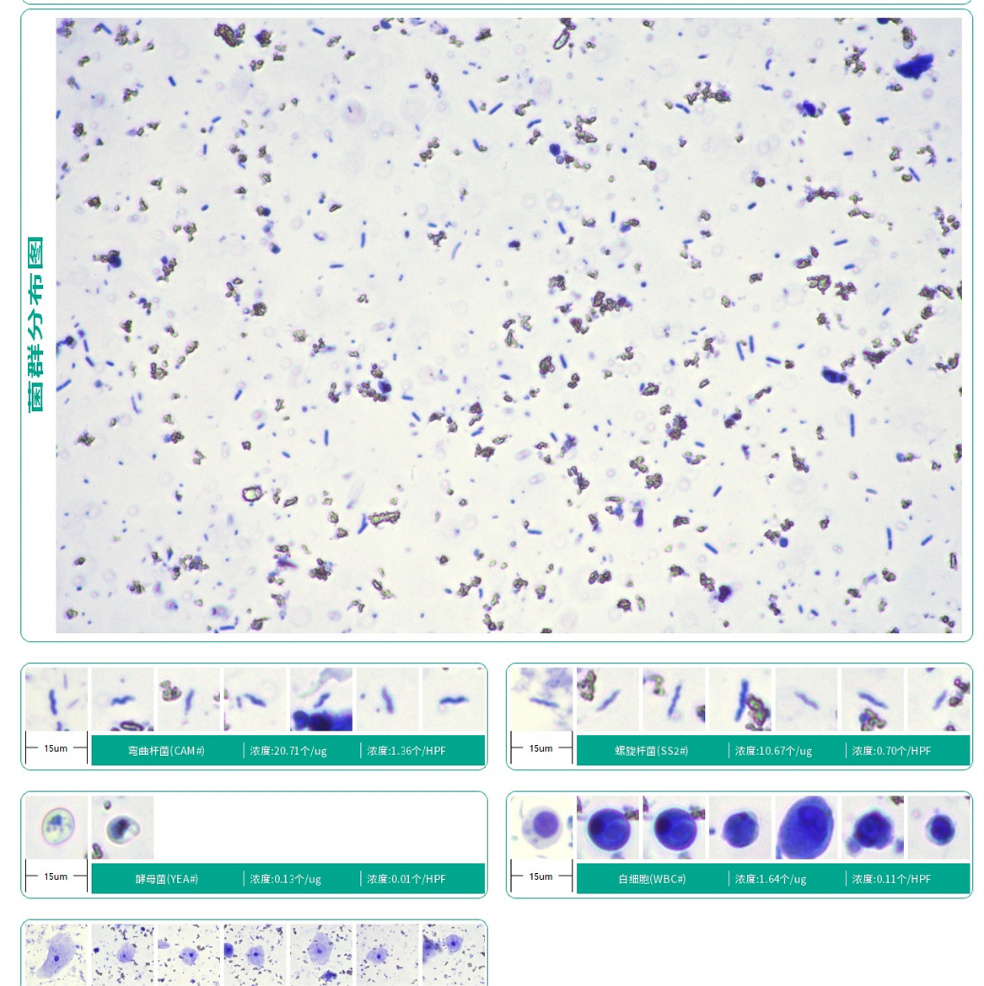
The dog presented with loose stool. Initial AI-assisted microscopy examination showed no significant abnormalities and indicated no parasitic infection.
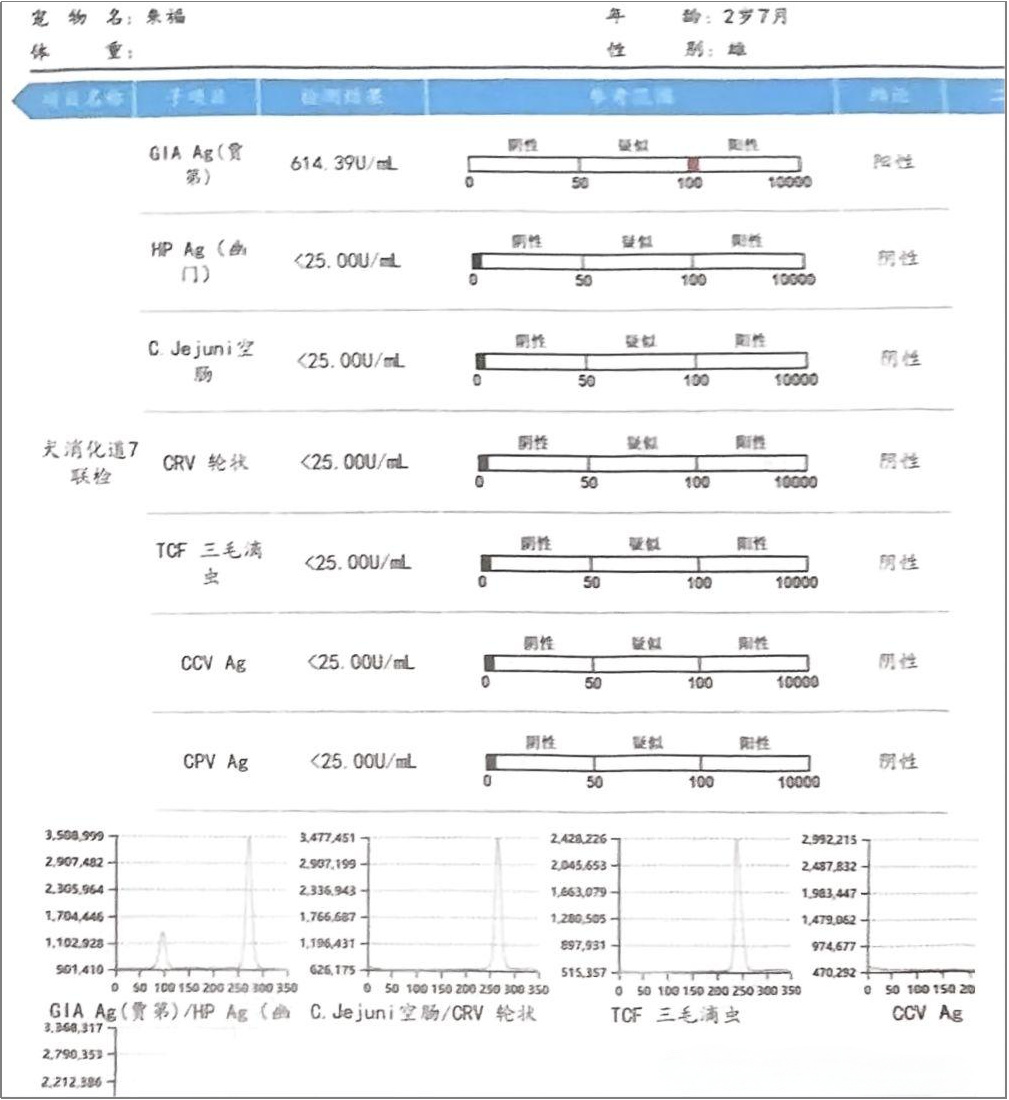
The New Test Gastrointestinal Tract Multiplex Panel subsequently detected a positive result for Giardia lamblia. The hospital was advised to treat the dog for Giardia infection. Meanwhile, fecal samples were sent for tripartite comparative verification, which confirmed a strong positive result for Giardia lamblia.
Follow-up treatment feedback: Following New Test’s accurate diagnosis and targeted therapy, the dog showed rapid clinical improvement and achieved full recovery.

Post time: May-29-2025




